Most policies make headlines for a day. A few rewrite how healthcare operates at its core.
The One Big Beautiful Bill, signed into law on July 4, is the latter. Its sweeping reforms around Medicaid eligibility, federal coverage pathways, and cost-sharing structures are set to affect every facility that relies on predictable reimbursements and claim integrity.
What sounds like a legislative milestone is, in practice, a direct operations challenge. And for many, the timelines are shorter than they appear.
This is where your facility’s audit, coding, and compliance strategy will either keep things stable or create ripple effects that impact revenue, care access, and patient satisfaction.
What the One Big Beautiful Bill Is Changing
The bill’s most visible changes fall into two categories: stricter Medicaid eligibility and verification rules, and expanded investment in rural care and telehealth. Together, these provisions are expected to reshape the payer mix, increase uninsured volumes, and introduce new risk areas for coding and claims.
Here is a snapshot of the most impactful changes:
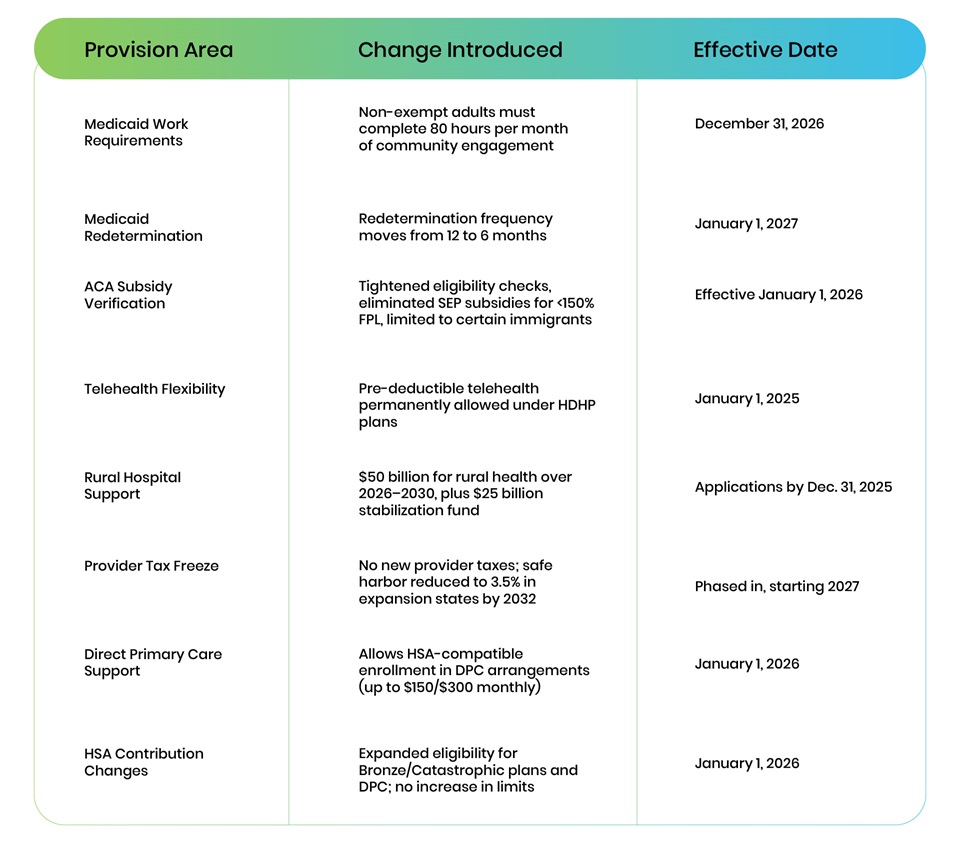
These changes are layered and complex. But one message is clear: coverage is shifting, and facilities need to prepare now.
Who Could Lose Coverage and What That Means for You
Will more people have access to care? Yes, but not all in the same way. The bill expands rural infrastructure, strengthens telehealth access, and reduces drug costs for patients who stay insured.
At the same time, the Congressional Budget Office (CBO) estimates that 7.8 million individuals could lose Medicaid coverage due to new work requirements and shorter redetermination cycles, with up to 16 million becoming uninsured by 2034 due to OBBBA and related policies.
What does that mean for healthcare facilities?
- Fewer covered visits, especially in rural and safety-net hospitals
- More uncompensated care and bad debt from uninsured patients
- Higher denial rates as documentation and eligibility rules tighten
- More complex billing workflows and greater risk exposure
How Facilities Can Prepare for the Coverage Shift
This is a moment where proactive planning can prevent downstream disruption. Healthcare organizations that invest in readiness now will be better equipped to safeguard revenue and maintain compliance as new provisions take effect.
Here are five core areas to prioritize:

- Validate Coverage Early and Repeatedly
Update your registration and billing workflows to verify eligibility with greater frequency and granularity. With six-month redetermination cycles, insurance status can change mid-treatment. Teams must be equipped to catch those changes in real time. - Strengthen Audit and Compliance Programs
Internal audits should not only focus on coding accuracy, but also surface recurring patterns in denials, eligibility issues, and claim rejections. A robust audit function can act as a predictive tool, helping teams flag risks before they escalate. - Train Coding Teams on New Risk Areas
As Medicaid and ACA rules evolve, coders need deeper visibility into how coverage intersects with documentation and code selection. Provide up-to-date training on payer-specific requirements, eligibility dependencies, and documentation best practices. - Track Policy Changes by State
Medicaid work requirements, redetermination frequency, and subsidy eligibility may vary significantly across states. Healthcare organizations should closely monitor state-level guidance and maintain flexible workflows that can adapt regionally. - Apply for Rural Investment Funds
Many small and mid-sized facilities will qualify for support from the bill’s $50 billion rural health allocation. But funding applications are time-bound and require detailed submissions. Eligible facilities should begin the application process as early as possible to avoid missing the December 31, 2025, deadline.
How LexiCode Supports Facilities During Healthcare Coverage Transitions
At LexiCode, we recognize that coding and compliance are foundational to maintaining both financial performance and care quality during times of regulatory change.
We support healthcare facilities with:
- Monthly audits of more than 50,770 medical records, uncovering risk areas before they become denials
- Annual coding volume of 15 million records, spanning inpatient, outpatient, and pro-fee services
- 98% coding accuracy, powered by certified coders and dual-level quality review
- Custom training for coding and provider teams, with CE credits and ongoing feedback loops
- Data-driven audit analytics that inform leadership, improve documentation, and reduce errors
- Cost optimization with offshore and AI-enabled coding solutions to reduce expenses without sacrificing quality
Balancing Cost Reductions with Operational Opportunity
Supporters of the One Big Beautiful Bill frame it as a tool for increasing efficiency, eliminating fraud, and realigning healthcare incentives. The bill introduces options like direct primary care, limits on duplicative coverage, and funding caps that aim to optimize federal spending.
But these efficiency goals come with tradeoffs.
Despite new rural investments and expanded telehealth access, the law still cuts more than $1 trillion in federal healthcare funding over the next decade. That shortfall is expected to push more responsibility onto providers, who will be asked to meet the same access and quality goals with fewer financial safety nets.
What Comes Next
The One Big Beautiful Bill healthcare coverage reforms will roll out over the next two years, with some provisions already in motion. With every new rule, the stakes for coding accuracy, billing integrity, and documentation rigor grow higher.
For healthcare facilities, the window to act is now.
Refining workflows, educating teams, and enhancing audit readiness today will reduce exposure later.
LexiCode can help your organization stay ready through every phase of this transition.
Let’s start the conversation about how we can support your team.